Herpes Drew a Scarlet Letter Across My Breasts
Latest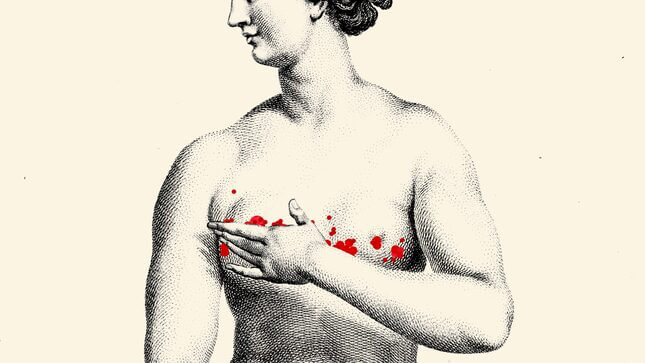
Graphic: Elena Scotti (Image: Wikimedia Commons)
“im coming thru on my way home for xmas. wanna grab a beer?”
It was a welcome text message. I was 23, new in town, and had just moved into a rickety apartment with two roommates and a cat named Theo. Our lopsided home was above a barbecue joint; it smelled perennially like pulled pork. I was a little lonely, a little uncertain. A visit from my not-quite-ex, never-really-was boyfriend would be a nice holiday distraction.
We had that beer. And another. Our feet found each other under the table; our hands sought out the familiar. He stayed over. It was fun and easy and years on, unmemorable. I don’t remember much of what we did, but I do remember that he nibbled my nipples.
A couple days after Christmas I started feeling sick. I drove back to my new apartment in a cold sweat and spent New Year’s in a feverish haze. After four days, my roommate pushed me to go to urgent care.
I sat behind a curtain, the cacophony of coughs ringing in my ears, and explained my symptoms: fever, sweats, feeling leaden all over. “There is one other thing,” I told the nurse practitioner. “I have this weird rash on my boobs.” She gestured for me to unhook my bra. It was freezing, but I complied, and pointed to the zit-like bumps ringing my areolas.
“Huh,” said the nurse practitioner, peering in as I drew back uncomfortably. “I’ve never seen that before.” She referred me to a dermatologist.
Of course, I thought. Of course.
I spent much of my childhood in dermatologists’ offices, doing battle with a severe case of eczema that wouldn’t quit. As I grew up, my skin largely cleared. Dermatological anomalies, I hoped, were relics of childhood. I was wrong.
-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-








































